AIDS stigma remains a problem in Ireland
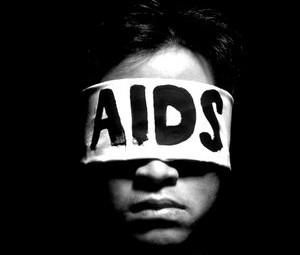
Today, 1 December 2009, is World AIDS Day. Figures released recently by St. James’s Hospital show a significant increase in new cases of the virus in Ireland for this year. While standards of treatment and prognosis are improving, surveys and anecdotal evidence show there is still a significant stigma attached to HIV and AIDS. This stigma is not only causing hardship to those with the disease, it is also preventing people from seeking tests and treatment for HIV.
In 2009, there has been a 20% increase in the number of new patients diagnosed with HIV infection in St. James’s Hospital, the highest number of new cases in one year since records began. The number brings the total number of HIV positive patients being treated by the Dublin hospital to approximately 2,000.
There has been a 100% increase in cases among ‘men who have sex with men’. Despite this, the greatest figures of HIV infection remain in the heterosexual population. The report shows rates of infection among intravenous drug users have reduced.
However, one of the most significant factors in treating and preventing HIV and AIDS is not medical care, but the issue of stigmatisation and discrimination still surrounding the diseases and experienced by HIV positive people in Ireland.
A 2008 report entitled “HIV Related Stigma and Discrimination in Ireland Today”, the first national report on HIV related stigma, reveals that ignorance and stigma surrounding HIV and AIDs remains strong in Ireland. The report was launched as part of the ‘Stamp Out Stigma’ campaign, a collaboration between the Department of Health, Irish Aid, non-governmental organisations focused on HIV and sexual health and people living with HIV. While the report found that the Irish public has a “notable level of sympathy and understanding towards those with HIV and AIDS”, some of the statistics it uncovered are shocking.
The report found:
- 23% of people would be worried about eating a meal prepared by someone with HIV
- 15% of those surveyed believe that those with HIV only have themselves to blame for their condition
- 49% of people living with HIV claim to have been discriminated against by their own friends and 28% by their own families.
- 43% have been discriminated against by their local community, 25% by social welfare and 18% by school or college.
- The report highlights “a considerable level of discrimination’ among the medical profession”, with 37% of people with HIV claiming to have been discriminated against by a doctor and 34% by a dentist.
- 84% of people with HIV feel that people with the virus are viewed negatively by society. However just 54% of the general public agree with this.
Ciaran McKinney, vice-chair of the ‘Stamp Out Stigma’ campaign, says that greater understanding of HIV is central to reducing stigma and that “the stigma uncovered in the studies clearly impacts on the health and wellbeing of those living with HIV”. Critically, such ignorance and stigma also acts as a deterrent to people coming forward for HIV testing, therefore constituting a key barrier to tackling HIV in Ireland.
James O’Connor, Membership Development Officer with Open Heart House, gave Politico some insight into the implications of the erroneous perception of HIV and AIDS has for Open Heart’s members. Open Heart House is Ireland's largest peer support network of HIV positive people. Open Heart House provides a range of programmes and services to support individuals living with HIV and AIDS and aims to challenge the social stigma and isolation of living with HIV through peer support.
Mr. O’Connor describes how, while the medical treatment of HIV and AIDS has excelled, “the stigma surrounding the diseases has not changed in twenty years.” In addition to self-stigma, HIV positive individuals face numerous challenges including ostracisation. Although Open Heart House, like many other non-government organisations, has seen a drop in its funding, they are in the final stages of preparing the Open Heart House Strategy for 2010-2014 and are confident that they will have the capacity to provide peer support to the rising number of HIV cases, in addition to their 900 existing members.
At the end of October, the Equality Tribunal delivered a ruling which represents a significant step towards the removal of stigma surrounding HIV, particularly in relation to medical treatment. In the case of Goulding v. O'Doherty, the tribunal ruled that Mr. Goulding, who is HIV positive, been denied a health service because of his HIV status. In her decision, the Equality Officer also highlighted the issue of misconceptions regarding persons living with HIV stating: "...persons living with HIV are often incorrectly perceived as being unhealthy or wrongly perceived as a threat to public health. It is crucial that these misconceptions are tackled effectively and immediately...".
However this ruling is just one step in the destigmatisation of HIV. A recent EU policy paper, ‘Combating HIV/AIDS in the EU and neighbouring countries 2009-13’, calls on governments and NGO’s to combat the spread of HIV by:
- improving information for all, especially targeting young people who have missed the successful HIV communication campaigns in the past
- addressing migrants from countries with a high prevalence of HIV to make them knowledgeable on preventing transmission, HIV testing and treatment options
- improving policies targeting, in particular, the populations most at risk, emphasising human rights, and addressing discrimination and stigma associated to HIV/AIDS
Government has Failed to Implement Strategy
HIV and AIDs are no longer the death sentences they were twenty years ago: developments in treatments mean that many people with HIV can expect to live to almost average life expectancy. Recent research in the US has even indicated that the development of a vaccine may not be far off. However, AIDS is still a fatal disease with no known cure.
In 2008 the Government published a report ‘HIV and AIDS Education and Prevention Plan 2008 -2012’. The action plan advocates placing a high priority on HIV testing for all target groups at risk of the disease, and progressive education and awareness campaigns to ensure accurate information is available to the public. However, the recently released figures indicate that investment in services and prevention strategies is inadequate and lacking the political will to be effective. Dublin AIDS Alliance has called on Government to resource the plan if it is to have any effect. And the executive director of the Dublin AIDS Alliance, Mary O’Shea, called for an intensive HIV/AIDS information and advertising campaign, similar to the graphic campaigns of the 1980s, coupled with the prioritisation of the national government health strategy on HIV infection.
The Alliance have further expressed concern that the current economic climate and funding cuts are placing a burden on already overstretched HIV/AIDS services and that any further reduction in such resources will have implications for public health in the future.
A Europe-wide survey release in Brussels in October reported that while health care and living conditions for people living with HIV/AIDS in Ireland are good, there is room for improvement. The Euro HIV Index 2009 ranked Ireland 10th out of 29 countries. The survey ranked Luxembourg in top position followed by Malta and Switzerland. “Ireland does rather well in all sub-disciplines of the Index, which is the reason for the 10th position in the ranking. However, there is room for improvement,” commented Dr Beatriz Cebolla, the Euro HIV Index Director.
HIV: A Global Problem
HIV and AIDS has had a devastating effect since the discovery of the virus in 1981. To date there have been 25 million deaths due to the disease. In 2007 there were 33.2 million people living with HIV and AIDS, 2.5 million new infections and 2.1 million deaths.
65% of all HIV and AIDS infections occur in Sub-Saharan Africa. HIV and AIDS are more prevalent in developing countries because poverty, malnutrition and HIV & AIDS are inextricably linked. Poverty can make a household more vulnerable to food insecurity and poor nutrition. It also leads to high-risk survival strategies like migration and prostitution, which increase the chances of contracting HIV.
Worldwide, young women are 1.6 times more likely than young men, to be HIV positive. This ratio is 3:1 in Sub-Saharan Africa.
Anti Retroviral Drugs (ARV) which can delay the development of HIV to AIDS by 20 years or more are expensive, and extremely difficult to obtain in some developing countries. Less than 30% of people living in low/middle income countries who are in need of immediate ARV treatment can access and afford it.
These issues are being exacerbated by the various crises of recent times. The sharp increase in food prices over the past two years has caused many starving HIV-positive patients in certain regions to abandon their ARV treatment as food prices rise. This carries the risk of drug resistance later. Increasing hunger is also fuelling increased risk-taking, such as prostitution, by individuals desperate to feed their children. Such high risk behaviour further fuels contractions of the virus.
HIV Global statistics:
- 33.4 million people living with HIV worldwide
- 31.3 million adults
- 15.7 million women
- 2.1 million children under 15
New HIV cases in 2007:
- 2.7 million people
- 2.3 million adults
- 430,000 children under 15
HIV-related deaths in 2007:
- 2 million total deaths
 Red Ribbons in support of World AIDS Day are available in certain outlets across Ireland including GAP, H&M and MAC counters and many university campuses.
Red Ribbons in support of World AIDS Day are available in certain outlets across Ireland including GAP, H&M and MAC counters and many university campuses.
Open Heart House pledges to provide confidential peer support nationally to those dealing with a HIV diagnoses. More information is available from the Open Heart House website.
